Introduction
Hypertension is the most common risk factor for cardiovascular diseases (CVDs).1 Globally it affects about 40% of the population and causes approximately 7.6 million deaths every year.2 Despite the availability of effective interventions, including antihypertensive medication only 20% with hypertension have well-controlled blood pressure.3 In Nepal, high blood pressure was the leading cause of CVDs in 20174 where 20–30% of adult women and men have hypertension.5 The high proportion of untreated (89% of those aware) and uncontrolled (96% of those on treatment) hypertension in Nepal,5 jeopardizes the government’s commitment to reduce CVDs.6
Management of hypertension may require substantial efforts, including adherence to antihypertensive medications, monitoring of blood pressure, frequent follow-up with healthcare providers, weight reduction, physical activity, healthy diet, and avoidance of alcohol and tobacco use.7 Patients with chronic conditions like hypertension often need social and family support to optimally manage their ailment.8,9 Social support is a multidimensional concept often defined as activities and relationships that individuals receive and provide to each other within their social networks.10 A large and diverse social support network can boost self-esteem and provide better access to information and resources.11,12 Health-related interactions with friends and family promote healthy behaviors including adherence to treatment.13–16 Feeling connected with others and the awareness that support is available when needed are important for positive health outcomes.17–19 Positive social relationships help patients cope with illness associated stress promoting better prognosis.20 Social support may protect patients from complications by helping with health management,16 or by encouraging healthy behaviors.21 However, the evidence on the role of social support in the management of chronic conditions is inconclusive. Studies have shown a positive,22–26 null27,28 and an inverse association29 between social support and management of chronic conditions. The role of social support in the management of chronic conditions like hypertension has not been sufficiently explored in the Nepalese context. One study from Nepal reported a positive association between social support and self-care for hypertension.30 In this study, we explored how perceived social support influences medication adherence and control of high blood pressure. The results from this study could serve to inform targeted community-based interventions according to the level of social support received by hypertension patients for controlling hypertension.
Materials and Methods
Study Setting
The study was conducted in Budhanilkantha municipality, Kathmandu, Nepal. The municipality has nearly 150,000 inhabitants31 and has 11 public health facilities that provide primary health care and tertiary care is provided by the private and public hospitals nearby. Hypertension prevalence of the urban areas such as Budanilakantha (25.2%) is similar to the national average (24.5%).5
Study Design and Population
Cross-sectional data collected at baseline from 1252 hypertensive individuals enrolled in a cluster randomized trial (Registration no: NCT05292469). The detailed trial methods are published elsewhere.32 Trained enumerators identified participants seeking support from health workers and volunteers, screened for eligibility, and obtained written informed consent after explaining the trial objectives. Eighteen years and older individuals with established hypertension diagnosis (systolic BP ≥140 mmHg and/or diastolic BP ≥ 90 mmHg on at least two consecutive visits or using antihypertensive medication) and able to respond to the questions were recruited. Pregnant women were excluded.
Data Collection
Trained enumerators collected baseline data from 2 May 2022 through 7 November 2022 using an android operating system tablet installed with KOBO toolbox electronic data collection platform. The questionnaire was pretested. Participants were shown picture cards with examples of physical activity and commonly used utensils for drinking alcohol to ensure accurate measurements.5
Outcomes
Hypertension control
An “Omron” digital instrument was used to measure blood pressure three times in a resting position and the mean of the last two measurements was registered. Participants with systolic and diastolic blood pressure less than 140 and 90 mmHg were categorized as controlled hypertension others as uncontrolled hypertension.
Medication adherence
We administered an eight-item Morisky Medication Adherence Scale (MMAS-8) (Supplementary Table 1).33 The scale is widely used to measure medication adherence and is reported to have good reliability (α = 0.83) and validity with sensitivity of 93% and specificity of 53% for low adherence.34 The first seven questions have responses YES coded as 0 and NO coded as 1. The code of the fifth question was reversed and the responses to the eighth question were re-coded from 2 to 0.75, 3 to 0.5, 4 to 0.25, 5 to 0 during the analysis. Responses to all eight questions were added to get MMAS, and a score above 6 was considered good adherence and ≤6 poor adherence.35
Exposures
Modified multidimensional scale of perceived social support (MSPSS) was used to measure the adequacy of support participants received from family, friends, and significant others (Supplementary Table 2).36 Twelve questions with answers on a 5-point Likert scale (1 = strongly disagree; 5=strongly agree) were asked to the participants. Cronbach’s alpha has been estimated to be 0.92, 0.85, 0.85 and 0.86 for total and family, friends, and significant others subscales, respectively.36 The MSPSS was translated into Nepali by SB and was reviewed by the study clinician. During training, the wording of the questions was discussed with the enumerators from the study community. The enumerators pretested the questions, and any problems encountered in administering the questions were discussed and addressed before finalizing the tool. The internal consistency reliability for the MSPSS was found good with a Cronbach’s alpha of 0.91 for the overall score and 0.87, 0.91, and 0.84 for family, friend, and significant other subscales, respectively. The overall MSPSS ranged between 12 and 60, high scores indicate high perceived social support. The subscale scores were calculated by adding the responses for related questions. During analysis, scores were divided by the number of questions included in each scale resulting in scores ranging between 1 and 5. The scores were categorized as low (1.00–3.59), moderate (3.60–4.59), and high (4.60–5.00) support.
Covariates
The covariates included in the model were age (continuous), gender (female/male), ethnicity (Brahmin Chettri/Newars/Tamang, Sherpa, Rai, Gurung, Magar/Dalits), current marital status (unmarried/married), education (illiterate/primary/secondary/high school and above), and per capita annual income in US dollars (continuous). Other variables considered were occupation status (unemployed/paid employment), self-reported diabetes status (status not known/non-diabetic/diabetic), years since hypertension diagnosis, and prescribed antihypertensives (Yes/No). The diet quality questionnaire assessed 32 different food groups participants ate in the 24 hours preceding the survey.37 The global dietary recommendation score (ranging from 0 to 18, higher score means better diet quality) was calculated by subtracting foods recommended to limit from foods recommended as healthy and adding nine. It measures adherence to a healthy diet protective against non-communicable diseases.37 Fruits and vegetable scores ranged from 0 to 6, with scores of <3 indicate the likelihood of eating less than 400 grams of fruits and vegetables.37 Daily salt intake was asked and categorized as ≤10 grams, 11–15 grams, and >15 grams. A global physical activity questionnaire38 was used to calculate metabolic equivalents of task (METs) minutes per week categorizing <600 METs (inadequate) and ≥600 (adequate). Body mass index of <25 kg/m2 and ≥25 kg/m2 was categorized as normal weight and overweight, respectively.39 Standard drinks per week were calculated by asking current alcohol drinkers about drinking frequency and amount of different types of alcohol5 and categorizing into non-drinkers (≤1 standard drink per month), moderate drinkers (<3 standard drinks per week), and high drinkers (≥3 standard drinks per week). Tobacco use including both smoked and chewed was categorized as never, and ever users.
Statistical Analysis
Descriptive statistics were presented as frequencies and percentages for categorical variables and mean and standard deviation for continuous variables. Confounders included in the model were identified a priori by constructing a directed acyclic graph (DAG)40 to assess the association between MSPSS and controlled hypertension and adherence to antihypertensives. We fitted Poisson regression to assess the association between MSPSS and hypertension control. Prevalence ratios and corresponding 95% confidence intervals were estimated. Two models were fitted, unadjusted (model 1) and adjusted for age, gender, ethnicity, marital status, education, and income (model 2). Similar models were also fitted to assess the association between MSPSS and adherence to antihypertensives. Based on the DAGs, mediators such as dietary, lifestyle and clinical factors were not included in the model. All analyses were performed with Stata 18.41
Ethics
We have obtained ethical approval from Nepal Health Research Council (Protocol number: 682/2021) approved on 24 December 2021 and Regional Committee for Medical and Health Research Ethics, Norway (Reference number: 399479) approved on 22 February 2022. We have adhered to the declaration of Helsinki throughout the research process.
Results
The mean age of study participants was 57.5 years, and 60% were females. Table 1 shows the distribution of sociodemographic, lifestyle and clinical factors by categories of overall MSPSS. Participants with high social support were generally younger and more often males, married, belonged to Brahmin/Chettri ethnicity, were highly educated, had paid employment, had high per capita income, physically active, overweight, drink <3 standard drinks per week, current tobacco users, consumed daily <10 grams salt, had high global dietary requirement score, consumed less fruits and vegetables, were diabetic, were prescribed more than three antihypertensives, had shorter duration since diagnosis of hypertension and had poorly controlled blood pressure.
 |
Table 1 Socioeconomic, Lifestyle, and Clinical Factors by Levels of Overall MSPSS |
Out of the 1252 participants 914 (73%) reported receiving moderate to high overall MSPSS. Figure 1 shows that the high proportion of individuals with controlled hypertension and good adherence to antihypertensives were in moderate MSPSS category (58.7%) and high MSPSS category (74.3%), respectively. The distribution of MSPSS subscales by status of hypertension control and adherence to antihypertensives are shown in Supplementary Tables 3 and 4.
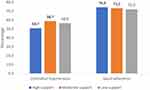 |
Figure 1 Proportion controlling hypertension and good adherence to antihypertensives in categories of overall MSPSS. |
Overall, there was no significant association between social support and controlled hypertension (Table 2). However, individuals who received a moderate level of social support from friends exhibited 1.18 (95% CI, 1.04–1.33) times higher prevalence of controlled hypertension compared to those receiving low support.
 |
Table 2 Association Between MSPSS and Controlled Hypertension |
Further, Table 3 shows that there was no association between social support and prevalence of adherence to antihypertensives, and unadjusted and adjusted estimates were very similar.
 |
Table 3 Association Between MSPSS and Adherence to Antihypertensives |
Discussion
In this study, we explored how perceived social support received by hypertension patients affected adherence to antihypertensives and control of hypertension. Our analysis showed that 73% of participants received moderate to high social support. Despite anticipating a positive association between MSPSS and controlled hypertension, we found that participants in the high MSPSS category had the lowest proportion of hypertension control (51%) while the proportion of good adherence did not differ between MSPSS categories. There was no association between MSPSS and adherence to antihypertensives and controlled hypertension except for friend’s sub-scale where higher prevalence of controlled hypertension was observed in moderate social support compared to low.
Very few studies from Nepal have reported on the relationship between social support and hypertension control and adherence to antihypertensives. Our finding that hypertensive patients receive high social support is in line with previous studies from Ethiopia42 and Turkey,43 but not with studies from Nepal30 and Malaysia.44 Previous studies from high-income countries agree with our findings that social support is neither associated with hypertension control45,46 (Spain/Korea) nor with adherence to antihypertensives28 (USA). However, a positive association between social support with controlled hypertension has been reported by a study from Vietnam47 and with adherence to antihypertensives by studies from India,23 China48 and Turkey.43 The inconsistent findings could be due to discrepancies in how social support was measured. A few studies have used MSPSS30,43,49 to measure social support but their outcome measure was self-efficacy to hypertension rather than hypertension control while those with hypertension control as the outcome measured social support differently by measuring frequency of visits by friends and family,45 social support inventory,28 self-esteem and belongingness23 and availability of informational, emotional, practical support.27,46,48
The quality and type of social support received has a bearing on adherence to medication and hypertension control.13 Practical support received for household chores lowered the risk of uncontrolled hypertension in Vietnam,47 whereas financial support from friends was harmful to adherence to medication in China.48 Therefore, nuanced studies disentangling the mechanisms through which social support the process of hypertension management are needed.
The reason hypertensive patients received high social support in our study may be due to availability of family members rendered by large family size in our sample. Despite the high level of support received by participants, we did not observe a significant positive association between MSPSS and hypertension control and adherence to antihypertensives. This may be due to a tendency of parents not wanting to burden children with their health concerns.50 Also, nearly 33% of the participants were illiterate and their friends and family are likely similar. Even when support is available, a poorly educated social network may not be capable of imparting the informational support needed to adhere to treatment and thereby control hypertension.51
Another explanation to the discrepancy of our results with other studies might be differences in individual and cultural characteristics. A large proportion of unemployed individuals may have skewed our sample towards a higher level of social support. People value financial support and therefore financially dependent individuals may report receiving high support. Also, the threshold for expected support may vary between different societies, for example in a patriarchal society like Nepal, women as primary care takers in the family may have a lower threshold of social support, whereas elderly men who command more respect in society may have a higher threshold.
We found a numerically higher prevalence of controlled hypertension among those receiving moderate support from friends but not those receiving higher support. A possible explanation might be that those receiving higher support spend longer time with friends and are thereby more exposed to peer pressure for unhealthy behaviour which was indicated as a barrier for effective control of blood pressure in our formative study in the same population.52 Reverse causation can also not be ruled out, as those with poorly controlled blood pressure may be receiving higher support from friends.
Strengths and Limitations
Our study adds to the sparse literature examining this association using validated instruments such as MSPSS and MMAS-8. We recruited hypertension patients from the community (not hospital) ensuring a representative sample. Since the outcome of interest (controlled hypertension and good adherence to antihypertensives) was common (larger than 10%), we fitted a modified Poisson regression model which gives a better approximation of the risk than overestimated odds ratio.53 This study is not without limitations. The cross-sectional design may have masked the true association between social support and controlled hypertension, as it is possible that individuals with uncontrolled hypertension or with poor adherence were receiving more support. Given the numerous statistical tests we conducted, it is essential to interpret any significant findings with caution to mitigate the risk of drawing false-positive conclusions. The findings are based on data from one urban municipality, which might limit the generalizability of our findings to the general hypertensive population in Nepal. Social support as a construct would be better explored using a mixed-method approach as the MSPSS tool does not capture the type of social support received.49 The reliance on self-reported data on medication and social support may have resulted in recall bias skewing the data in the direction of social desirability leading to over-estimated adherence and social support.
Conclusion
This study shows that hypertensive patients in Nepal in general have good social support.
However, social support was not foremost for medication adherence and control of hypertension. Future interventions for example digital technologies that facilitate remote monitoring and communication with care providers54 should nurture the high level of social support received by the hypertension patients. However, contextual studies to delineate the mechanisms through which social support can augment adherence to treatment, healthy behaviour, routine monitoring, and follow-up for hypertension management are needed for social support to have precedence in future interventions for hypertension patients.
Abbreviations
CVDs, Cardiovascular diseases; DAG, Directed acyclic graph; METs, Metabolic equivalents of task; MMAS, Morisky medication adherence scale; MSPSS, Multidimensional scale of perceived social support.
Data Sharing Statement
Data cannot be shared publicly for ethical reasons but are available on reasonable request to Ms Sanju Bhattarai and Dr Abhijit Sen.
Acknowledgments
We would like to thank all the participants in the study. We would like to thank field researchers Ms Apsara Basnet, Ms Geeta Tripathi, Ms Pema Tamang, Ms Prasoon Pandey, Mr Kishore Adhikari, Ms Sarita Bhandari, Ms Supriya Kharel.
The MMAS-8 Scale, content, name, and trademarks are protected by US copyright and trademark laws. Permission for use of the scale and its coding is required. A license agreement is available from MMAR, LLC., www.moriskyscale.com.
Funding
This work was supported by Norwegian University of Science and Technology, Trondheim, Norway (Project number 981023100).
Disclosure
The authors declare that they have no competing interests in this work.
References
1. Roth GA, Johnson C, Abajobir A, et al. Global, regional, and national burden of cardiovascular diseases for 10 causes, 1990 to 2015. J Am Col Cardiol. 2017;70(1):1–25. doi:10.1016/j.jacc.2017.04.052
2. Lawes CM, Hoorn SV, Rodgers A. Global burden of blood-pressure-related disease, 2001. Lancet. 2008;371(9623):1513–1518. doi:10.1016/S0140-6736(08)60655-8
3. Chow CK. Prevalence, awareness, treatment, and control of hypertension in rural and urban communities in high-, middle-, and low-income countries. JAMA. 2013;310(9):959. doi:10.1001/jama.2013.184182
4. Bhattarai S, Aryal A, Pyakurel M, et al. Cardiovascular disease trends in Nepal – an analysis of global burden of disease data 2017. IJC Heart Vasculature. 2020;30(100602):100602. doi:10.1016/j.ijcha.2020.100602
5. Dhimal MBB, Bhattarai S. Report of non communicable disease risk factors: STEPS survey Nepal 2019. Kathmandu; 2020.
6. Collaborators NC, Stevens GA, Mathers CD. NCD countdown 2030: worldwide trends in non-communicable disease mortality and progress towards sustainable development goal target 3.4. Lancet. 2018;392(10152):1072–1088. doi:10.1016/S0140-6736(18)31992-5
7. Prevention, detection, evaluation, and treatment of high blood pressure the seventh report of the joint national committee on complete report. U.S. Department of Health and Human Services, National Institutes of Health, National Heart, Lung, and Blood Institute, National High Blood Pressure Education Program; Contract No.: 04-5230; 2004.
8. Barth J, Schneider S, von Känel R. Lack of social support in the etiology and the prognosis of coronary heart disease: a systematic review and meta-analysis. Psychosomatic Med. 2010;72(3):229–238. doi:10.1097/PSY.0b013e3181d01611
9. Eom C-S, Shin DW, Kim SY, et al. Impact of perceived social support on the mental health and health-related quality of life in cancer patients: results from a nationwide, multicenter survey in South Korea. Psycho-Oncology. 2013;22(6):1283–1290. doi:10.1002/pon.3133
10. Tardy CH. Social support measurement. Am J Community Psychol. 1985;13(2):187–202. doi:10.1007/BF00905728
11. Scanfeld D, Scanfeld V, Larson EL. Dissemination of health information through social networks: twitter and antibiotics. Am J Infect Control. 2010;38(3):182–188. doi:10.1016/j.ajic.2009.11.004
12. Perry BL, Pescosolido BA. Functional specificity in discussion networks: the influence of general and problem-specific networks on health outcomes. Social Networks. 2010;32(4):345–357. doi:10.1016/j.socnet.2010.06.005
13. DiMatteo MR. Social support and patient adherence to medical treatment: a meta-analysis. Health Psychol. 2004;23(2):207–218. doi:10.1037/0278-6133.23.2.207
14. Trivedi RB, Ayotte B, Edelman D, Bosworth HB. The association of emotional well-being and marital status with treatment adherence among patients with hypertension. J Behavl Med. 2008;31(6):489–497. doi:10.1007/s10865-008-9173-4
15. Cornwell EY, Waite LJ. Social network resources and management of hypertension. J Health Social Behav. 2012;53(2):215–231. doi:10.1177/0022146512446832
16. Gallant MP, Spitze GD, Prohaska TR. Help or hindrance? How family and friends influence chronic illness self-management among older adults. Research on Aging. 2007;29(5):375–409. doi:10.1177/0164027507303169
17. Callaghan P, Morrissey J. Social support and health: a review. J Adv Nurs. 1993;18(2):203–210. doi:10.1046/j.1365-2648.1993.18020203.x
18. Bolger N, Zuckerman A, Kessler RC. Invisible support and adjustment to stress. J Pers Soc Psychol. 2000;79(6):953–961. doi:10.1037/0022-3514.79.6.953
19. Norris FH, Kaniasty K. Received and perceived social support in times of stress: a test of the social support deterioration deterrence model. J Pers Soc Psychol. 1996;71(3):498–511. doi:10.1037/0022-3514.71.3.498
20. Idler EL, Boulifard DA, Contrada RJ. Mending broken hearts. J Health Social Behav. 2012;53(1):33–49. doi:10.1177/0022146511432342
21. Ford CD, Sims M, Higginbotham JC, et al. Psychosocial factors are associated with blood pressure progression among African Americans in the Jackson Heart Study. Am J Hypertens. 2016;29(8):913–924. doi:10.1093/ajh/hpw013
22. Taher M, Abredari H, Karimy M, Abedi A, Shamsizadeh M. The relation between social support and adherence to the treatment of hypertension. J Educ Community Health. 2014;1(3):63–69. doi:10.20286/jech-010348
23. Padhy M, Lalnuntluangi R, Chelli K, Padiri RA. Social support and adherence among hypertensive patients. AJHM. 2016;1(1):33–40.
24. Pan J, Hu B, Wu L, Li Y. The effect of social support on treatment adherence in hypertension in China. Patient Preference Adherence. 2021;15:1953–1961. doi:10.2147/PPA.S325793
25. Osamor PE. Social support and management of hypertension in south-west Nigeria: cardiovascular topic. Cardiovasc J Afr. 2015;26(1):29–33. doi:10.5830/CVJA-2014-066
26. Sabaté E, World Health O. Adherence to long-term therapies: evidence for action. World Health Organization. 2003;194.
27. Adisa R, Olajide OO, Fakeye TO. Social support, treatment adherence and outcome among hypertensive and Type 2 diabetes patients in ambulatory care settings in southwestern Nigeria. Ghana Med J. 2017;51(2):64–77.
28. Hm ST, Quyyumi A, Reilly C, Pemu P, Dunbar S, Dunbar S. The relationship among health beliefs, depressive symptoms, medication adherence, and social support in African Americans with hypertension. J Cardiovasc Nurs. 2019;34(1):44–51. doi:10.1097/JCN.0000000000000519
29. Uchino BN. Understanding the links between social support and physical health: a life-span perspective with emphasis on the separability of perceived and received support. Perspectives Psychol Sci. 2009;4(3):236–255. doi:10.1111/j.1745-6924.2009.01122.x
30. Acharya R, Chaudhary A, Pandey J, Pandey C. Self-Care Management And Its Associated Factors Among Patient With hypertension in Nepal. J Chitwan Med Coll. 2022;12(2):91–96. doi:10.54530/jcmc.637
31. Karki M Budhanilakantha municipality profile; 2019.
32. Bhattarai S, Shrestha A, Skovlund E, Åsvold BO, Mjølstad BP, Sen A. Cluster randomised trial to evaluate comprehensive approach to hypertension management in Nepal: a study protocol. BMJ open. 2023;13(5):e069898. doi:10.1136/bmjopen-2022-069898
33. Morisky DE AA, Krousel-Wood M, Ward HJ, Ward HJ. Predictive validity of a medication adherence measure in an outpatient setting. J Clin Hypertens. 2008;10(5):348–354. doi:10.1111/j.1751-7176.2008.07572.x
34. De M Concurrent and predictive validity of a self-reported measure of medication adherence; 1986.
35. Lee GKY, Wang HHX, Liu KQL, Cheung L, Morisky DE, Wong MCS. Determinants of medication adherence to antihypertensive medications among a Chinese population using morisky medication adherence scale. PLoS One. 2013;8(4):e62775. doi:10.1371/journal.pone.0062775
36. Stewart RC, Umar E, Tomenson B, Creed F. Validation of the multi-dimensional scale of perceived social support (MSPSS) and the relationship between social support, intimate partner violence and antenatal depression in Malawi. BMC Psychiatry. 2014;14(1). doi:10.1186/1471-244X-14-180
37. Global diet quality project – DQQ tools & data. [Internet]. Available from: https://www.globaldietquality.org/dqq. Accessed March 21, 2024.
38. Global physical activity questionnaire Global Physical Activity Questionnaire (GPAQ). [Internet]. Available from: www.who.int/chp/steps. Accessed March 21, 2024.
39. World Health Organization. GLobal status report on non communicable diseases 2014; 2014.
40. Textor J. Adjustment criteria in causal diagrams: an algorithmic perspective. In Proceedings of the 27th Conference on Uncertainty in Artificial Intelligence (UAI 2011) [press release]; 2011.
41. StataCorp. Stata Statistical Software: Release 18. College Station, TX: StataCorp LLC; 2023.
42. Ademe SAF, Gela D, Gela D. Hypertension self-care practice and associated factors among patients in public health facilities of Dessie town, Ethiopia. BMC Health Serv Res. 2019;19(1):1–10. doi:10.1186/s12913-019-3880-0
43. Rabia Hacihasanoglu Asilar AY, Saglam R, Demirturk Selcuk E, Erduran Y, Sarihan O. The effect of loneliness and perceived social support on medication adherence self-efficacy in hypertensive patients: an example of Turkey. Eur J Cardiovasc Nurs. 2020;38(4):183–190.
44. Nur Syafaah Nazeri NM, Redzuan M, Abdul Mulud Z. Social support and self-care practice among patients with hypertension in a teaching hospital. Malaysian J Med Health Sci. 2021;18(8):281–290.
45. Redondo-Sendino PG-C Á, José RB, Rodríguez-Artalejo F, Rodríguez-Artalejo F. Relationship between social network and hypertension in older people in Spain. Rev Esp Cardiol. 2005;58(11):1294–1301.
46. Jiwon Baek NWH, Chang Kim H, Youm Y, Youm Y. Sex-specific effects of social networks on the prevalence, awareness, and control of hypertension among older Korean adults. J Geriatric Cardiol. 2016;13(7):580–586. doi:10.11909/j.issn.1671-5411.2016.07.005
47. Luu Quang Thuy NHT, Hong Trung L, Huy Tan P, et al. Blood pressure control and associations with social support among hypertensive outpatients in a developing country. Biomed Res Int. 2021;2021:1–10.
48. Bingjie Shen TG, Xinyu D, Chenyang P, Zhao J, Liu Y, Liu Y. Medication adherence and perceived social support of hypertensive patients in China: a community-based survey study. Patient Preference Adherence. 2022;16:1257–1268. doi:10.2147/PPA.S363148
49. Hatah ELK, Ali AM, Mohamed Shah N, Islahudin F, Islahudin F. The influence of cultural and religious orientations on social support and its potential impact on medication adherence. Patient Prefer Adherence. 2015;9:589–596. doi:10.2147/PPA.S79477
50. Acharya TDG, Traille K, Dhakal H. Senior citizens in Nepal: policy gaps and recommendations. Gerontol Geriatr Med. 2023;9:23337214231179902.
51. Isa MD, Shahar SHF, He FJ, Majid HA. Associations of health literacy with blood pressure and dietary salt intake among adults: a systematic review. Nutrients. 2021;13(12):4534.
52. Bhattarai S, Bajracharya S, Shrestha A, et al. Facilitators and barriers to hypertension management in urban Nepal: findings from a qualitative study. Open Heart. 2023;10(2):e002394. doi:10.1136/openhrt-2023-002394
53. Spiegelman D. Easy SAS calculations for risk or prevalence ratios and differences. Am J Epidemiol. 2005;162(3):199–200.
54. Kario K, Nomura A, Harada N, et al. Efficacy of a digital therapeutics system in the management of essential hypertension: the HERB-DH1 pivotal trial. Eur Heart J. 2021;42(40):4111–4122. doi:10.1093/eurheartj/ehab559
