Equity and emergency care was the theme for day two of the 21st International Conference on Emergency Medicine, on 17 June.
Dr Sarah Simons, an emergency medicine registrar in Naarm/Melbourne, live-tweeted the discussions from @WePublicHealth as part of Croakey Conference News Service coverage of #ICEM22.
Below is a selection of her tweets. In the second half of the post are some wrap-up reflections from conference participants.
Despite concerns aired at the conference about workforce burnout, Simons observed, “the enthusiasm, storytelling, connections and engagement at this conference offer a lot of cause for optimism”.
Stay tuned for more stories to come, and follow this Twitter list, including more than 110 ICEM presenters and participants.
Sarah Simons tweets:
Why equity matters
The session was chaired by Dr Simon Judkins and Dr Ffion Davies, with a panel discussion facilited by Dr Clare Skinner.
Global health equity and the social determinants of health: the African experience
Dr Mulinda Nyirenda opened the plenary session talking about her experiences as an Emergency Physician in Malawi.
Access to care, system resilience and investment and funding in emergency care continue to be pertinent issues in Africa – more recent investment in resuscitation resources in particular has lead to a spike in better outcomes.
@MulindaNyirenda speaks about how the social determinants of health are increasingly prevalent in emergency care in Malawi, more so than with routine checks or elective care and even more relevant when looking at the challenges between rural and metropolitan healthcare access.
Emergency care in Malawi is primary care; staffing shortages and more broader resource limitations implicate access to healthcare; 40 percent of @MulindaNyirenda’s work is emergency resuscitation medicine but the remainder is often more primary care based.
NCDs are increasingly prevalent in Africa, especially hypertensive emergencies and strokes. Emergency care cannot be only for the rich.
Pursuing health equity for asylum seekers and displaced persons across the globe
Kon Karapanagiotidis, CEO and founder of the Asylum Seeker Resource Centre, said: “We have politicised what is a health and human rights issue… The heroes of every story are the refugees – those who fight, risk their life, dignity every day.”
There are still more than 200 refugees in Nauru living in squalor, but despite governmental failings, Karapanagiotidis speaks of the courage and compassion of the Australian public to uphold the human rights of refugees by protesting and blocking exits to hospitals to prevent deportation.
Health is a human right. Ahmed was 24 when he died of a foot infection in Nauru.
He talks about how @ASRC1 doubled down to keep doors open and cover medicines, supply food all through the pandemic. COVID mortality rates for Greek people in Melbourne are eight times higher than the general population – 13 times higher for Middle Eastern people.
So what if we cared for people before the crisis really begins? Prevention is better than cure.
Development of gender equity and equality systems in emergency medicine
Imron Subhan, India and Priyadarshini Marathe, United Kingdom
@imronsubhan and@PRIYAMARATHE10 speaking on the development of gender equity and equality systems in emergency medicine. “We’re here to make you uncomfortable. How does your patient’s gender matter in the ED?”
@imronsubhan has five minutes and one message: gender equality is not solely a woman’s problem. Sex and gender must be embedded early into our health curricula. Biases are introduced when medicine is taught as universal and unisex.
“Teaching gender equity and equality should be like basic life support” – lifesaving and not optional.
Dr Priyadarshini Marathe: Practical everyday tips and tricks for addressing biases and inequity: flagging biases on a ward round; create a WhatsApp group as a safe space with peers (for example, female colleagues in your workplace) to listen, empathise and share knowledge and experience.
Write yourself a couple of stock answers for educating peers and challenging interactions “it sounds we are at a different stage of learning about this”. Recommended reading with books/novels directing to lived experiences.
Equity, First Nations Peoples and healthcare
Professor Greg Phillips now shares insights from his 25 year career in equity and healthcare for First Nations people.
He describes 60,000 years of thriving First Nations culture, science, art, politics, geology, medicine and law long preceding colonisation in Australia.

Recognising privilege and white fragility on an individual and systematic level in healthcare is vital for health equity. It can be extremely confronting to have this pointed out to us as clinicians who genuinely believe we are always trying our best for our patients.
Aboriginal representation at every level and in every discipline is vital, as is rewriting health curricula and integration of culture.
How does our advocacy shape and influence future healthcare?
Professor Phillips references the legacy of the late Professor Paul Farmer who spoke about how the practice of medicine should not be about benevolence, but instead about social justice.
Health inequities in African American and Latin American communities: challenges and solutions
Dr Gillian Schmitz talks about health inequities in the USA, using COVID as an example of disparities in housing, transport, employment and diet influencing health and access to care for African American and Latin American communities.
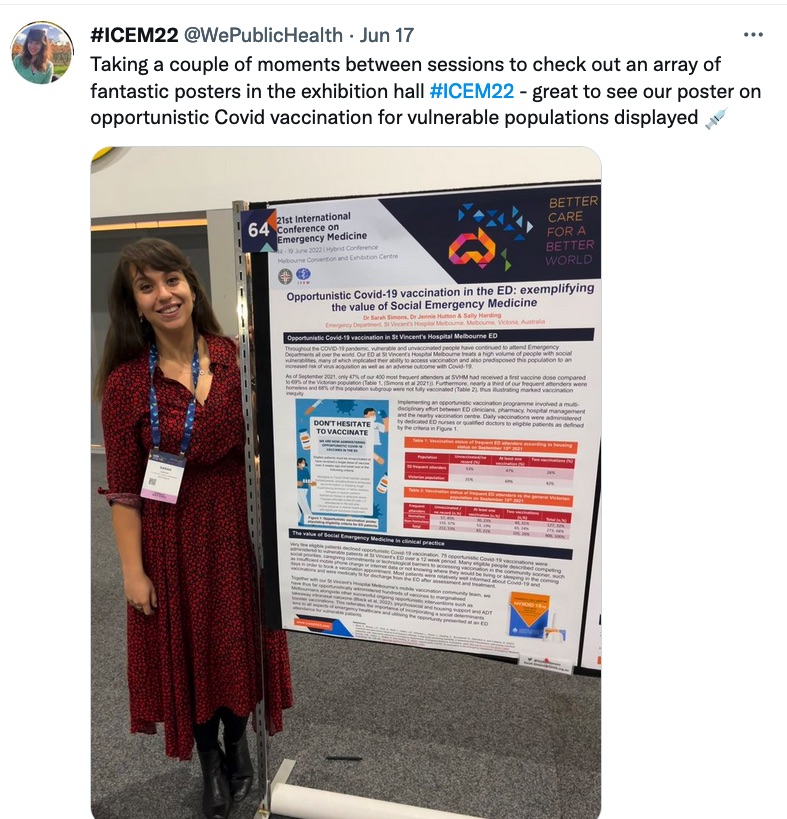
This reinforces the need for screening in the ED: HIV, hepatitis, STIs as well as smoking cessation & opportunistic vaccinations for flu and hepatitis. Teaching communities about communicable diseases with appropriate language and translation provision is paramount.
@GillianMD1 also talks about firearm violence in the US, a subject that many Australian emergency clinicians are very fortunate to have limited experience of and a pertinent example of how health and political action are directly intersecting and implicated.
Indigenous health service equity
First up of the breakout sessions was Dr Glenn Harrison chairing a discussion on Indigenous health service equity.
Dr Inia Tomash was first up from Auckland, sharing his national research project on examining inequalities in Aotearoa NZ EDs with patient centred markers of care and mortality. Māori people are known to be high users of ED services with room for improvement of care.
Retrospective review of NZ ED admissions 2006-2012: 5.9 million presentations in total. After repression analyses and control for confounders, ED mortality and representation after ED discharge was significantly higher for Māori population, suggesting different patterns in ED usage between Māori & non-Māori people – younger, more deprived, longer triage time.
Tomash’s top tips for redressing ED inequity: accept that this a problem that needs addressing and that puts patients at risk. We can start by quantifying our own biases and develop our critical consciousness.
The mindset of “going overboard for difficult patients” needs to change; this should instead be normalised as the gold standard! Use the resources available and engage with local Indigenous health units, practitioners and liaison officers.
Innovation in First Nations dermatology
Crystal Williams and Gabrielle Ebsworth
Gabrielle Ebsworth told us about her important work with the First Nations dermatology clinic. What started as a small rural telehealth service last February is now a dedicated successful face to face and telehealth service for and by First Nations people with easy, open referral processes and patient engagement. Demand currently far exceeds current resources and funding.
There are only four First Nations dermatologists in Australia, all of whom have only become fellows in the last two years. Part of the clinic’s work includes a monthly journal club for Victoria GPs to promote education, awareness and improve quality of referrals.
@g_ebsworth is very clear though – @TheRMH team don’t want this to be a national service. Aboriginal communities are not homogenous. Every region deserves and needs to have their own doctors and specialised services. More info is here.
Overcoming racism and bias
Gina Bundle, senior Aboriginal Health Liasion officer @thewomens
Gina spoke about her lived experience of the legacy of the Stolen Generations, how she ensures the hospital is held to their apology to protect every First Nations woman and baby and keeps their promises.
Creating an environment that First Nations people can walk into and know that they feel safe is incredibly important – the presence of Indigenous artwork and possum skin cloaks in a healthcare setting is so much more than decoration.
Part of Gina’s role is to keep her colleagues’ diaries updated with important First Nations calendar events all year round. National Sorry Day is so more than just a march; she wants colleagues to visit their offices, seek advice and share experiences long after NAIDOC week.
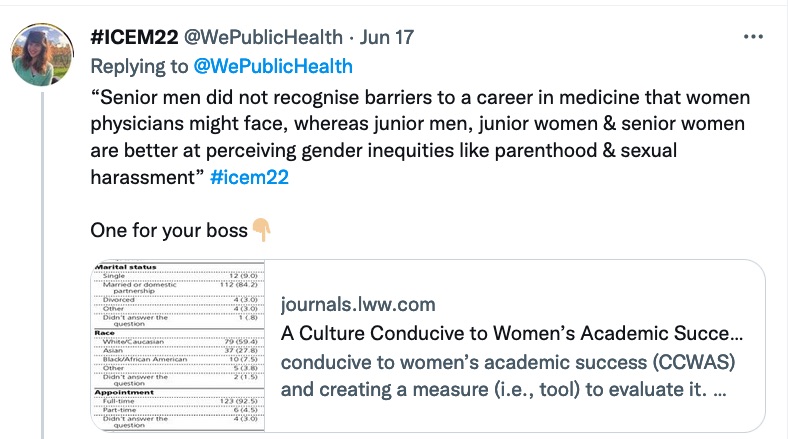
Development of gender equity and equality systems
Gender equality in EM – where do we stand today?
Dr Sally McCarthy says we still have some way to go – a brief glance at the predominantly female audience here speaks volumes about our approach to improving gender equality in EM and shows we have a long way to go still.
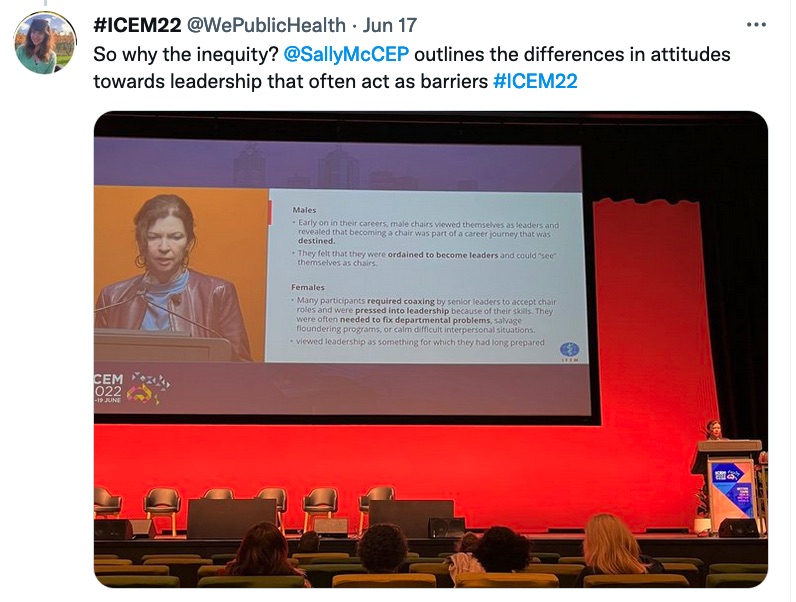
 See the article mentioned above here.
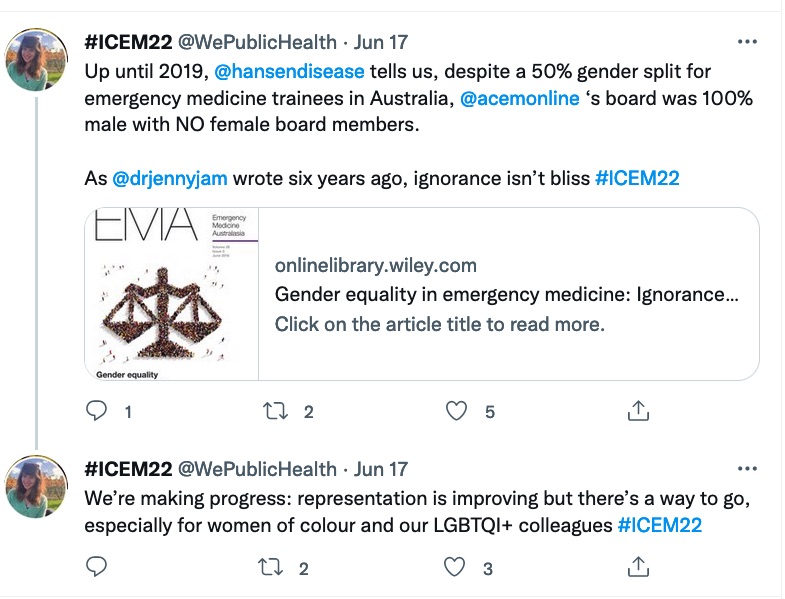
See the article mentioned above here. 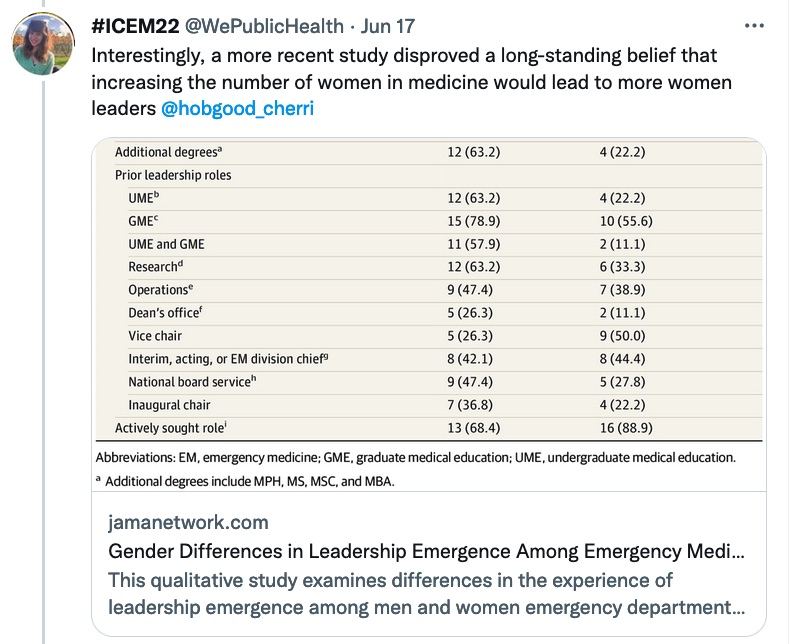 See the JAMA article here.
See the JAMA article here.
Persistence of gender inequality in developed countries – why?
Dr Gayle Galletta talks about the persistence of gender inequality in developed countries, sharing her experiences as an American Emergency Physician in Norway.

Taking women leadership to the next level – the 2.0 move
Dr Kim Hansen

Equity through advocacy
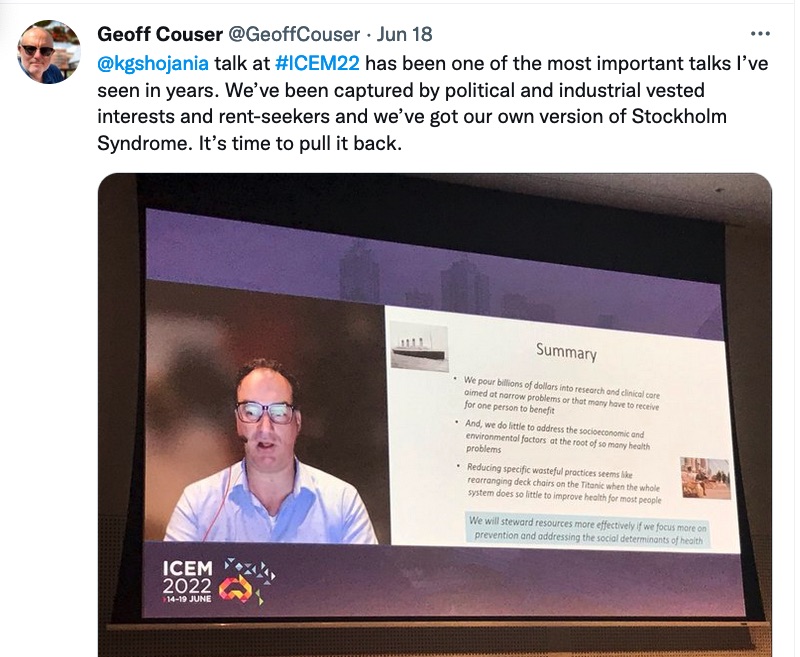
The role and power of research
Professor Brendan Crabb – @CrabbBrendan – shares about how research can be integrated into community care in order to build capacity and self sustained progression in emergency healthcare.
He describes the malaria incidence as an example – barriers to malaria are both technical and non technical requiring a variety of approaches. Research is a powerful tool of hope and a valuable a starting point to implement real, physical change.
The role and power of politics and advocacy for emergency care from the Tuvalu perspective
Dr Aloima Taufilo, Tuvalu
Wise words and inspirational efforts from @ATaufilo as she reflects on the power of social media communication to maintain and strengthen not only health literacy but political relationships to advocate for more than 2,000 Tuvali people with COVID last year.
Societal racism feeds into health system, clinician and patient factors – doctors often take cognitive shortcuts in decision making processes, with challenges including time constraints, multi tasking, need for closure, stress and sleep deprivation.
The role and power of education
Professor Papaarangi Reid, Aotearoa/New Zealand, talks about the power of education. A key message of COVID was to “listen to the scientists” but this proved insufficient; the science also needs political will and social capital to get anywhere.
The role and power of the media
Jo Chandler, Australian journalist
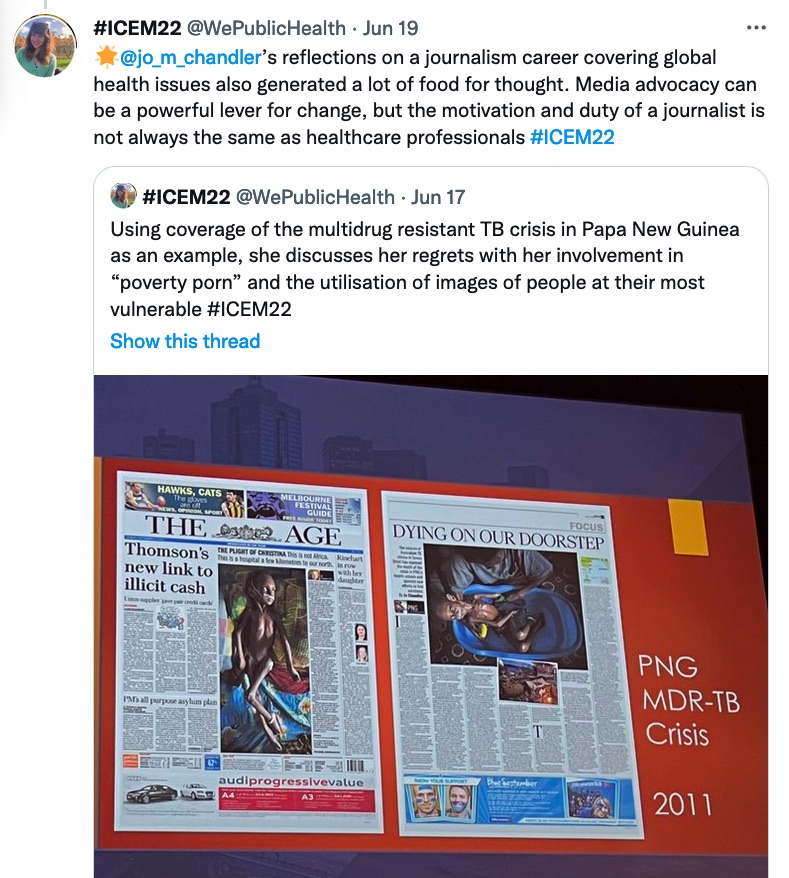
“Did it make a difference?” It can be difficult to know without a parallel universe, but shortly after publication an urgent and reactive mobilisation of resources and funding was injected into PNG.
How do we weigh up the risks of media advocacy and subsequent media exposure to advocate for vulnerable people? A great audience question from Dr Georgina Phillips in our advocacy plenary.
@jo_m_chandler answers that one blessing of social media is immediate engagement w educative, practice changing and informative feedback in real time. Longevity of journalistic relationships is also vital to build relationships and share narratives without damaging consequences.
The role and power of professional advocacy
Dr Dinesh Palipana shares his story with our audience – half way through university, he acquired a life changing spinal cord injury in a car accident. He found himself negotiating a minefield of challenges related to his disability & went on to complete medical school
He tells us how the ability to advocate for others reflects an immense position of privilege. Our titles and positions as doctors afford us great authority and privilege. Sometimes we don’t dare to speak up, for fear of reprobation, loss of status, vanity or fear.
“The biggest mistake a physician can make is to treat someone’s body but not their soul.” We have a responsibility to our communities, to acknowledge our privilege and to speak up with courage and make powerful people feel uncomfortable.
Dr Jenny Jamieson concludes today’s events, describing how Emergency Medicine sits at the coalface of society, combining science, sociology, anthropology and health.
In my view, the enthusiasm, storytelling, connections and engagement at this conference offer a lot of cause for optimism.
A final point: as emergency doctors we’re used to life and death situations, and many of us learn how to detach when things get tough for our own psychological self preservation. We need to be empathetic with humanity and humility but burnout is real. How do we find the balance?
Trainee matters
The author at work
Final conference reflections
As the conference wound up, participants shared reflections.


Thanks tweeps!
The Croakey Conference News Service team acknowledges and thanks #ICEM22 participants for their engaged and contributory tweeting.
According to Symplur analytics, 1,287 Twitter accounts engaged with the hashtag, sending 9,689 tweets and creating 88.2 million Twitter impressions during the period 10-22 June.
See the Twitter transcript.
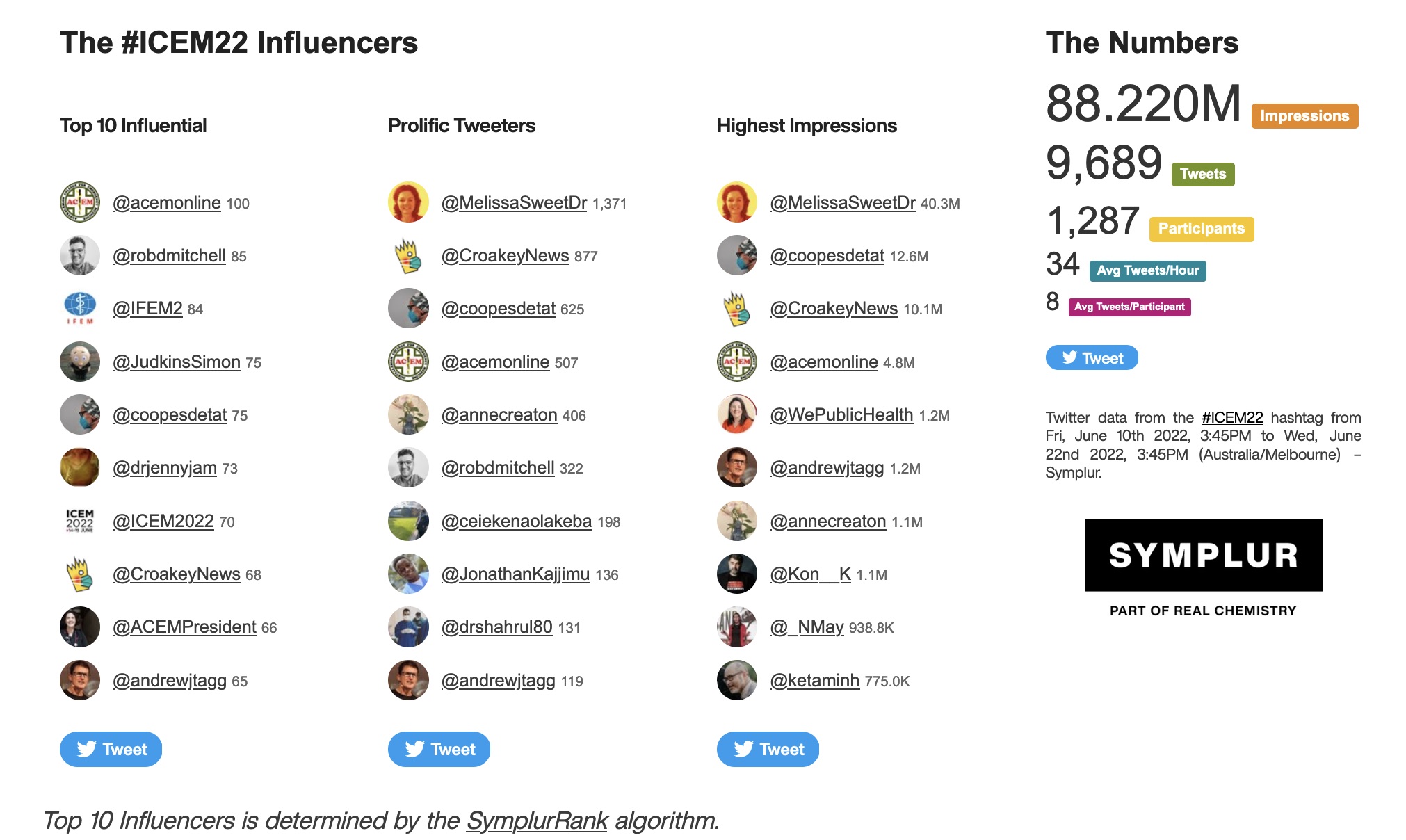
 The hashtag also trended on 16 June.
The hashtag also trended on 16 June.
Follow this Twitter list of #ICEM22 presenters and participants, and bookmark this link to track coverage by Croakey Conference News Service.
